What you Need to Know About your Osteoporosis Meds

Menopause can naturally bring about a lot of physiological changes for women. Around 7 out of 10 women experience things like sleep disturbances, hot flashes, depressed mood, and anxiety. These changes take place due to the natural decline in hormone levels because the body is entering a phase in life when reproductive hormones are no longer as necessary. Unfortunately, menopause-related hormone declines can also mean a heightened risk of osteoporosis.
When a female is determined to have low bone density or osteoporosis, most physicians take the route of prescription medications aimed at preventing bone damage. However, addressing the root cause of the problem with HRT (hormone replacement therapy) may be the more viable option for treatment. Let's take a closer look at osteoporosis, bone density changes during menopause, and more.
During the first decade of menopause, most women will lose about two-thirds of their natural bone mass. Typically, the more significant loss will occur between one and three years after the onset of menopause. Unfortunately, the changes in bone density can mean the bones get more brittle and easier to fracture. Sometimes, the bones will become so brittle that simply too much stress will cause them to break or fracture.
Women usually reach their peak bone mass at about the age of 30, and, for the most part, that density stays about the same all the way through menopause. Bone cells naturally regenerate on their own, but this process takes about three months to complete. In fact, every year, about 10 percent of bone cells have regenerated for the average adult. However, when the natural hormones start to wane due to menopause, the bone regeneration rate changes.
Why Estrogen Is Important to Your Bones
Estrogen is actually heavily used during the bone cell regeneration process. This one hormone is related to:
-
Initiating bone regeneration
-
Promoting the reduction of the cells that degrade bone (osteoclasts) and reducing resorption of the bones
-
Preventing the breakdown of the cells that build bone (osteoblasts)
The demineralization process still occurs with low estrogen levels, but the remineralization rate slows when blood estradiol levels drop. Therefore, bones can get weaker relatively quickly. Progesterone, another hormone that can drop during menopause, is also important to support the formation of new bone.
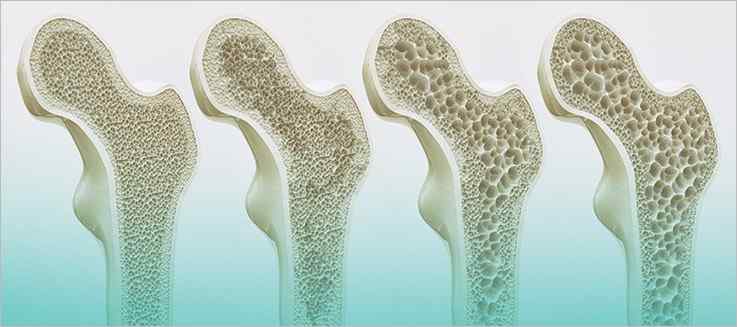
When the rate of demineralization exceeds that of regeneration, bones become weaker and less dense. The initial stage of this action is often diagnosed as osteopenia. Osteopenia is almost like the beginning phases of osteoporosis, even though not every woman diagnosed with osteopenia will be diagnosed with osteoporosis.
While the bone mass density lowers with osteopenia, the bones may not necessarily be easier to break or substantially brittle; there is only a notable change in density. Osteoporosis, however, is diagnosed when the bone mass density (BMD) reaches a point when the bones are substantially more porous and much more likely to sustain damage. A woman with severe osteoporosis may even sustain a fracture by coughing too hard, bending over, or even hitting a part of their body against a ledge or wall.
How are bone density problems diagnosed?
Bone density problems are diagnosed by doing a bone density test. These tests are designed to get an accurate measurement of both the strength of your bones and bone mass. A dual-energy x-ray absorptiometry, referred to as a DEXA scan, is most commonly used for diagnosis. The test looks at bone density in different parts of the body, such as in the wrists, hips, and spine, and then assigns a score referred to as a T-score.
If you have a T-score between -1 and -2.5, you may be diagnosed with osteopenia. If you have a T-score below -2.5, you will be diagnosed with osteoporosis.
What is a normal bone density for women?
The normal bone density for women is a T-score of -1.0 or above. For example, if you have a T-score after a DEXA scan of -0.9 or even 0, you will be considered to have normal bone density levels. The lower the score goes, the more porous and more prone to breakage the bones are as well.
Can you rebuild bone density once it's lost?
Bone density can be improved to some degree for most women with osteoporosis, as long as the condition is diagnosed early and the proper steps are taken. Usually, doctors recommend:
-
Exercise
-
A healthy diet with ample daily calcium (1,500 to 2,000 mg) and vitamin D (1,000 to 2,000 IU)
-
Quitting excessive alcohol consumption and smoking
-
Taking osteoporosis medications
Many people have specific concerns about certain parts of their bodies when it comes to low bone density. You may be asking, "How can I increase the bone density in my spine, or how can I increase the bone density in my hip?" Essentially, you will want to follow the same tips for rebuilding bone or supporting bone remineralization, regardless of the specific part of your skeleton you are most concerned about. However, you may want to try targeted exercises that can strengthen the bones in that part of your body.
Research has shown that women with the lowest bone density levels and the greatest risk of fractures usually also have the lowest estrogen levels. The biggest underlying cause of osteoporosis for postmenopausal women is estrogen deficiency, so hormone replacement therapy (HRT) seems to be a highly viable option for treatment.
Several studies have examined the effectiveness of HRT for bone density problems. One study found that women receiving HRT had fewer fractures than those who were given a placebo. An assessment of other available studies shows that HRT is associated with 30 percent fewer fractures for women with bone loss issues related to osteoporosis.
HRT for deterring bone loss can pose several benefits. One, HRT doses don't have to be all that high for a female to see the bone-protective effects. Some women may be good candidates for a low-dose estrogen and progesterone, for example, which would offer bone-protective qualities without a lot of side effects. Studies have even shown that ultra-low estrogen doses may protect the integrity of the bones in women over the age of 60 who may be looking to avoid things like breast tenderness or stimulation of the endometrial system.
One other notable advantage of HRT for bone loss is the fact that the medication may help deter some of the undesirable symptoms of menopause in addition to helping to protect the bones. So, if a woman is in the earlier stages of menopause when symptoms may be at their worst and bone loss is most likely to rapidly occur, that woman may only need to take HRT to help with deterring both issues.
While HRT does show promise for supporting and protecting bone density, many physicians will take the more traditional approach of prescribing medications. Several types of medications may be prescribed for either osteopenia or osteoporosis. Here is a look at some of the most common medications and the risks and benefits of each.
Bisphosphates
Biophosphates like Fosamax, Reclast, and Boniva are the most common type of medication prescribed for osteoporosis. This medication is formulated to prevent bone loss and can help prevent both spinal and hip fractures. However, the medications do not come without risks. Bisphosphates may involve side effects like:
-
Photosensitivity
-
Flu symptoms
-
Headaches
-
Bone pain
-
Sore mouth
-
Digestive upset
Unfortunately, bisphosphates may also occasionally lead to painful fractures in the upper femur after long-term use. And, there is some speculation that taking the medication for the long term can increase your risk of certain types of cancer.
Prolia
Prolia is an injectable medication that belongs to a group of medications known as monoclonal antibodies. Monoclonal antibodies are formulated to destroy certain cells in the body in an effort to protect or preserve healthy cells. In the case of osteoporosis, Prolia actually inhibits ligands that normally signal osteoclasts to kick off the demineralization process. While the medication can be effective, some people can be more prone to fractures when they stop taking the medication. Plus, Prolia can be linked to musculoskeletal pain, serious skin infections, and even urinary tract infections.
Forteo
Forteo is one of the only prescription medications approved by the FDA that actually rebuilds bone, and this medication is one of the most newly available. So far, this medication is approved for use for two years and is only available as an intravenous injection. While the medication can be effective for rebuilding bone for post-menopausal women, Forteo is related to some pretty serious side effects, such as:
-
Back spasms
-
Leg cramps
-
Depression
-
Hypercalcemia
-
Heightened risks of bone cancer
Forteo is also not a good fit for every patient. Anyone who is at risk of cancer, has high calcium levels in the blood, has undergone radiation therapy, or has had kidney stones should not take Forteo.
Osteoporosis and bone density loss can be especially concerning for women. If you have been diagnosed with either osteopenia or osteoporosis, it is important to get a good look at your options. If you have questions about HRT versus other osteoporosis medications, be sure to discuss the pros and cons of each with your pharmacist. Both medications may come along with risks, but HRT may be the more logical option in many cases. Reach out to us at Harbor Compounding Pharmacy to find out more about osteoporosis medication options.



