Fight PCOS, Diabetes, and Infertility with Myoinositol

Polycystic Ovarian Syndrome (PCOS) is a relatively common issue that affects as many as 5 to 10 percent of women during their childbearing years. Some researchers speculate that even though PCOS is common, as many as 50 percent of women with PCOS are not diagnosed or never seek medical advice for their issues.
While PCOS is mostly associated with difficulties in getting pregnant, women with PCOS often struggle with specific hormonal imbalances and metabolic issues that can bring along a host of other problems. Unfortunately, many of the current treatments aimed at PCOS only help with certain symptoms. However, certain natural PCOS supplements are generating quite the buzz in the medical community and are demonstrating a high degree of effectiveness.
Research is shedding more and more light on the pathophysiology behind PCOS and our understanding has grown substantially over the past few years. What we already knew was that there are two specific factors that are usually at work: heightened androgen levels and higher levels of insulin in the blood.
Androgens are essentially hormones most often associated with men, such as testosterone and DHEA. Women who have PCOS are usually found to have higher than normal androgens than what would be normal for most females which contributes to things like acne, facial har and oily skin.
Insulin is responsible for converting food into energy. However, women with insulin resistance don't respond properly to the natural insulin hormone their bodies provide. In turn, insulin levels in the blood get high, blood sugar levels are unstable, and the woman has a risk of developing type 2 diabetes.
What we didn’t know before that we know now is that high insulin levels are responsible for causing an imbalance of certain cellular messengers called inositols by effecting a key enzyme called epimerase. The imbalance of inositols and their messages is thought to be at the crux of the situation, providing a new target for therapy.
PCOS and Diabetes
Since women who have PCOS have problems with insulin resistance, about 40 percent of those who are diagnosed with PCOS will eventually be diagnosed with diabetes. Women who are overweight, don't eat healthily or get enough exercise, or who have a history of diabetes in their family are more likely to have insulin resistance along with PCOS. While it can seem that insulin resistance and reproductive issues would be worlds apart, hormonal issues are behind both problems. So, having problems with both is common.
The symptoms of PCOS can be unique to a woman as well as which hormonal imbalances may be at play. For example, PCOS hirsutism (excess hair growth), may be more common for a woman with PCOS who has excessively heightened levels of testosterone. Some generalized symptoms may include:
- Irregular menstrual cycles - Women with PCOS may miss periods, have fewer than eight periods a year, stop having a period altogether, or have periods more often.
- Weight gain or difficulty losing weight - PCOS weight gain can be directly related to insulin resistance or high levels of androgens.
- Acne - PCOS may lead to acne on the upper back, chest, or face.
- Skin darkening - The skin may darken under the breasts, in neck creases, or in the groin area.
- Hair thinning - Hair loss in the pattern of male-pattern baldness can occur with PCOS.
- Abnormal hair growth - About 70% of women with PCOS have PCOS facial hair or hair growth in unusual parts of the body where men normally grow hair.
- Skin tags - Skin tags may show up in the neck area or in the armpits.
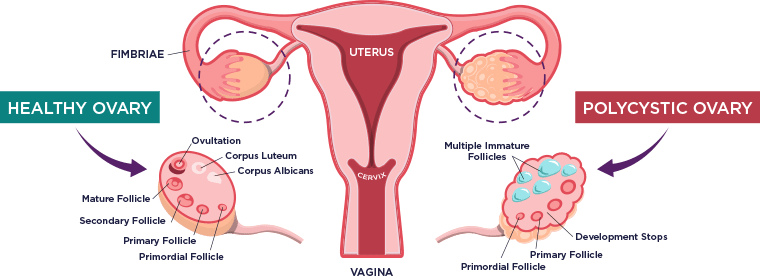
One of the main reasons women with PCOS seek medical advice is because they find it more difficult to get pregnant. This is because inositol imbalance brought on by insulin resistance and androgen excess can throw off one of the main hormones responsible for stimulating your cycle, FSH (follicle-stimulating hormones) and estradiol.
The hormonal imbalance that comes along with the condition can interfere with the typical ovulation patterns, which means your chances of getting pregnant with PCOS will be lowered. Women with PCOS, however, do still get pregnant and finding the right treatment which can “Normalize” your ovulation cycles is vital.
Unfortunately, PCOS doesn't go away on its own and there is no real cure for the condition. While women may reach a certain age beyond their reproductive years when they may not be as affected by unstable ovulation, the problems with heightened insulin resistance and high androgen levels can still pose problems. Therefore, the health risks that can come along with PCOS are an issue for women for the rest of their lives. Even though PCOS is considered a female issue that can cause detrimental effects far beyond the reproductive years, the right treatment plan can deter health risks and improve your quality of life for the long term.
The most typical PCOS treatments revolve around attempting to alleviate some symptoms associated with the condition. In many cases, doctors will recommend certain lifestyle changes and prescribe medications. While both lifestyle changes and the commonly used medications can offer some improvements, none of these options will actually address every aspect of the condition.
Prescription Medications for PCOS
Three primary medications are commonly prescribed for PCOS: metformin, birth control, and clomiphene.
Birth control is often prescribed to help “stabilize” (not “normalize”) your menstrual cycle. Birth control, however, works by suppressing hormones and ovulation and will most likely not help in any endeavors to increase fertility or help with the underlying insulin resistance and androgen excess.
Clomiphene is a medication often prescribed to stimulate ovulation. Up to 80 percent of women who take clomiphene do begin to ovulate and 30 to 40 percent of women will become pregnant. Clomiphene and fertility treatments, however, will not correct your underlying metabolic disorder, and usually comes at great monetary expense often exceeding tens of thousands of dollars.
Metformin, which is a common type 2 diabetes medication, encourages sugar uptake on a cellular level to keep blood glucose levels at a more stable state. Since metformin can help with hyperinsulinemia, it can also help to slowly correct the hormonal imbalances at play. Metformin, however, can cause deficiencies in vitamin B12, and must be addressed since these deficiencies can lead to higher homocysteine levels, which is a risk factor for heart disease.
Anti-androgen medications that block male hormones may also be prescribed for women beyond their child-bearing years to deter some negative symptoms like excess hair growth. These medications, however, are only meant to address symptoms of the disease and will not address the root cause.
Lifestyle Changes for PCOS
Some evidence suggests that dietary changes, exercise, and weight loss may help with some PCOS symptoms. For example, a doctor may recommend that you lower carb and sugar intake, increase cardio exercise, and try to lose a percentage of your body weight. One study found that losing just five percent of body weight may improve issues with insulin resistance, fertility, and hormone levels. Another study found that weight training three times a week for four months led to reduced testosterone levels and blood sugar levels among 45 women with PCOS.
Inositol for PCOS is growing to be a highly noteworthy option for women who have been diagnosed with PCOS. One reason that is the case is inositol may actually target the underlying issues at play with the condition, which in turn can alleviate most of the symptoms associated with PCOS.
What Is Inositol Exactly?
Inositol is a molecular carbohydrate, which happens to be a natural component in cellular membranes within the body and very similar to glucose. This particular molecule is not only naturally found in the cells of mammals but is also found in certain foods, such as beans, citrus, and cantaloupe. Inositol can be either Myo-Inositol (MI) or D-Chiro-Inositol (DCI). Inositol has a number of jobs within the body, including mediating bodily responses to certain hormones.
The Science Behind Myo-Inositol for PCOS
Because inositol plays such a big role in how the body responds to hormones in the body, the molecule may also help women with PCOS. When inositols are introduced to cell membranes in the body, they become the precursory messenger for both insulin and FSH (follicle-stimulating hormones). If there are some unknown defects in the pathway for these functions, there can be an impairment in insulin signaling that leads to insulin resistance. Therefore, an introduction of more inositol through supplements may help with PCOS.
Research into the effectiveness of myoinositol has been especially promising. One study involved 25 participants with PCOS and issues with infertility. Of the 25 participants, 88 percent had restored menstrual cycles, 72 percent achieved normal ovulation, and 40 percent actually became pregnant after treatment with Myo-inositol combined with folic acid for six months.
In a controlled clinical study performed in 2013, the 50 overweight patients with PCOS actually underwent a hormonal evaluation and glucose tolerance test before 12 weeks of therapy and then again after treatment with Myo-inositol and folic acid. In all patients, insulin and testosterone levels were reduced after treatment and menstrual cycles were restored.
A comparative study published in 2017 also found that a combination of myoinositol and folic acid seemed to be as effective for PCOS as treatment with metformin. In that particular comparative study, both groups had similar beneficial outcomes: serum progesterone levels dropped, pregnancy rates increased, and menstrual cycle disorders seemed to stabilize. It is worth noting that even though both metformin and myoinositol may have similar efficacy, myoinositol is related to far fewer and far less worrisome side effects.



